The following is a guest article. Their opinions and statements are entirely their own. Information on the writer, Doc Martyn, can be found at the bottom of the article.
Medical Bytes Thailand No 101: “82% of medical diagnoses can be made on history alone”
Published 16/12/2023
1. The story as told by Gary, Jess’s father: Jess, aged 26, started to feel a kind of pressure in her lower right abdomen about three weeks ago (roughly 20 Nov). The feeling of pressure (and of something swelling inside her) continued to increase. Just over a week ago, it started to feel painful and uncomfortable. She did not have a fever.
On Friday (1 Dec) it became acute. She went to BKK hospital, Chiang Mai. The doctor said it may be appendicitis or ovarian cysts or kidney stones. They would have to do a CT scan. Because of the cost (฿17,000), Jess went to the ER at Nakornping (a government hospital), where they did a CT scan and blood tests. They said there was some sign of an infection, but no appendicitis (or anything else).
By Tuesday, her condition had not improved. She did not want to try yet another random hospital doctor. She sought out a Thai GP who seemed to have some experience with women’s health and gynaecological issues. The female doctor prescribed a painkiller and two antibiotics, Cobay and Amoxiclav, for a Urinary Tract Infection, a UTI.
After another couple of days (Thursday 7th), there was no improvement. So, she tried the Ram Private Hospital in Chiang Mai. The doctor said he could not see everything on the CT scan, in particular the ovaries were obscured. He needed to do an ultrasound. (Author’s comment: The ovaries were clearly visible on the CT scan! An Ultrasound was not required. Keep the money rolling in!) Jess was told she had PID, Pelvic Inflammatory Disease. She was instructed to stop the antibiotics for her UTI. She was given an antibiotic intravenously (Ceftriaxone) and prescribed Metronidazole (400mg 3X/day) and Doxycycline (100mg 2X/day).
After 5 days, the urine culture test ordered by the GP showed no UTI.
On Sunday, because she could not get any answers over the phone, Jess returned to the Ram Hospital with her urine test results. She was told to come in to speak to the doctor. But instead, another doctor re-examined her. The new doctor suggested that it may be a muscle condition and wanted to prescribe painkillers. He did mention that she did have ovarian cysts, but they are very small. They charged her ฿1000, despite telling her that there would be no charge for discussing the previous consultation.
So, as feared, another runaround and wild goose chase and no wiser!
2. Gary contacted me last Sunday to seek my opinion. He sent me the aforementioned story. Extrapolating from this medical history only, the medical misadventure in this case becomes evident.
3. A. The initial differential diagnosis; Appendicitis, Ovarian Cyst or Kidney Stones:
-Initially, Appendicitis causes pain around the navel. As the illness progresses the pain moves to McBurney’s point, see photo 1 (Cover photo) Further, once infected the appendix deteriorates rapidly, usually within 2-3 days, producing a fever and significant debility. The protracted nature of Jess’s illness, the distribution of her pain and the absence of fever were not consistent with Appendicitis.
-Ovarian cysts are usually asymptomatic. Occasionally, they may cause bloating and lower abdominal pain and/or lower back pain. Jess’s pain was not typical Ovarian cyst pain.
-Kidney Stones cause acute severe intermittent colicky pain which radiates from the flank into the groin. Jess’s pain was not typical of Renal Lithiasis.
Thus, Jess’s pain was not caused by any of these conditions.
B. The GP’s diagnosis of UTI: Jess did not have urinary frequency, dysuria (painful urination), or cloudy urine. She did not have a UTI, yet she was given strong antibiotics.
C. PID causes fever, vaginal discharge and lower abdominal/pelvic pain. The diagnosis of PID was erroneous, yet her antibiotics were changed in accordance with the new diagnosis.
4. Jess’s medical story indicated that she did not have an infection of any sort. The ‘long-standing’ discomfort, 2 weeks, in the right side of her lower abdomen suggested either a colonic, large bowel, problem or pathology of the pelvic organs. She was not constipated. The onset of acute pain on December 1st suggested a ruptured right sided ovarian cyst. This provisional diagnosis was made solely from her symptoms.
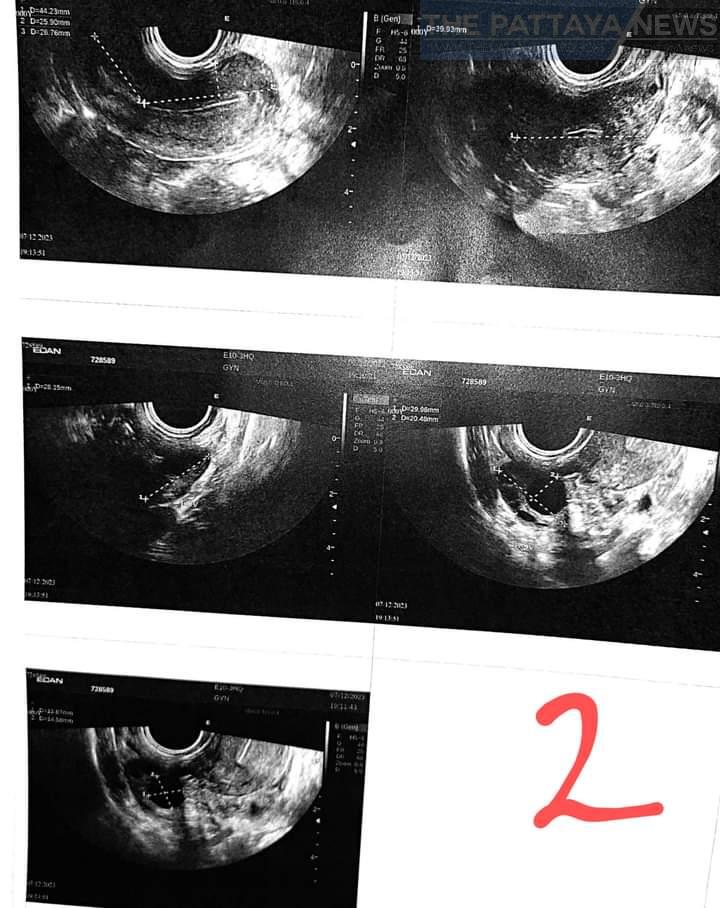
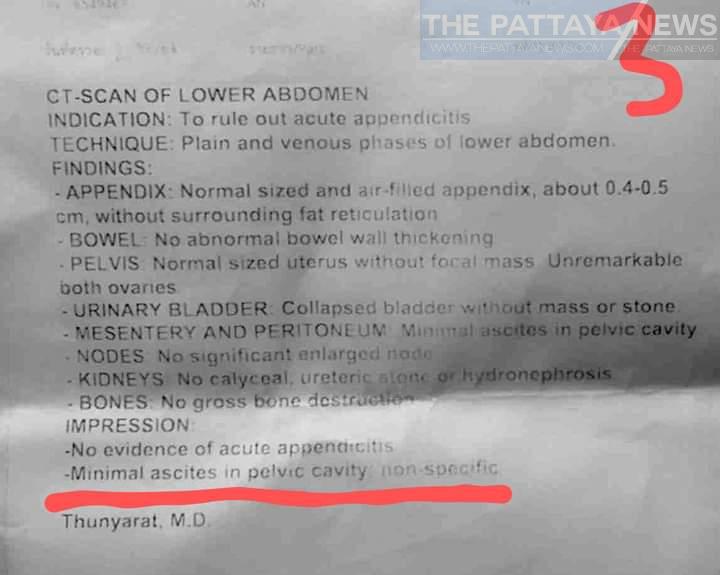
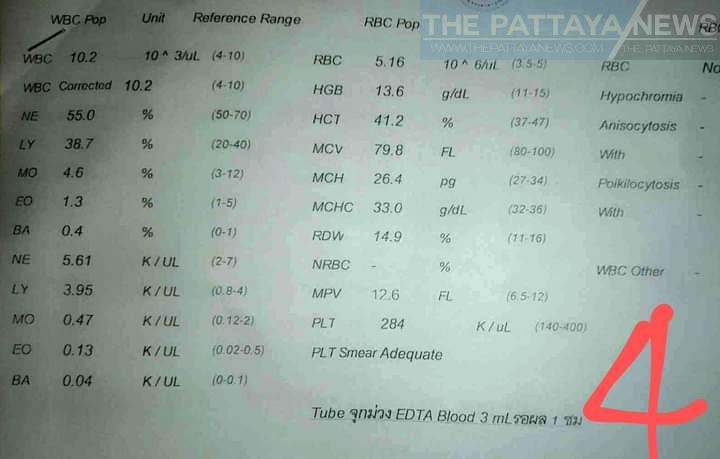
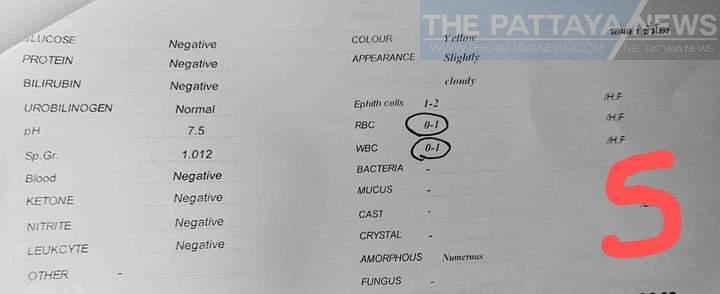
5. Her pathology and radiology results, which arrived the following day, confirmed the provisional diagnosis. The CT scan of her pelvis indicated that she had a ruptured right sided ovarian cyst, see photo 2 with ascites, fluid, in her pouch of Douglas, see report 3. Her other tests confirmed that she did not have a blood infection, see photo 4, nor a bladder infection, see photo 5, nor PID.
6. Jess was seen by five different Thai doctors who, despite having the patient in front of them with her pathology and radiology results, not one was able to identify this, relatively easy, diagnosis.
7. What confirmed the diagnosis was the last comment on the report of Jess’s CT scan: ‘Minimal ascites in pelvic cavity, nonspecific’. Ascites is a build-up of fluid in the abdominal cavity. In Jess’s case it was fluid in the pelvic cavity, aka the Pouch of Douglas. This fluid came from her ruptured right sided ovarian cyst. Five Thai doctors missed, or ignored, this significant radiological finding. This suggests that these five Thai doctors did not understand the implication of non-specific pelvic ascites.
For many years, I have written about the poor standards of Thai Medical Education. As discussed in previous MBT posts, Western Medical Colleges consider the Thai medical school education to be inadequate. Thai trained doctors are not allowed to practice medicine in the west without additional training and examination.
That said, there will be no change in the deficiencies of Thai trained doctors, as seen in this MBT, unless and until each Thai doctor is held personally responsible, with a pecuniary penalty, for their errors.
8. “82% of medical diagnoses can be made on history alone” (Ref: JR Hampton: Relative contributions of history-taking, physical examination, and laboratory investigation to the diagnosis and the management of medical outpatients: BMJ, May 1975.)
Addendum: Over the past 6 years, as a retired medic living in Buriram I offered second opinions on any medical issue. I recently moved to Pattaya. As in this case, if you reside outside of Pattaya, telephone consultations are provided. For assistance; please contact me, Doc Martyn, on Facebook or call Dao on 095 414 8145.




